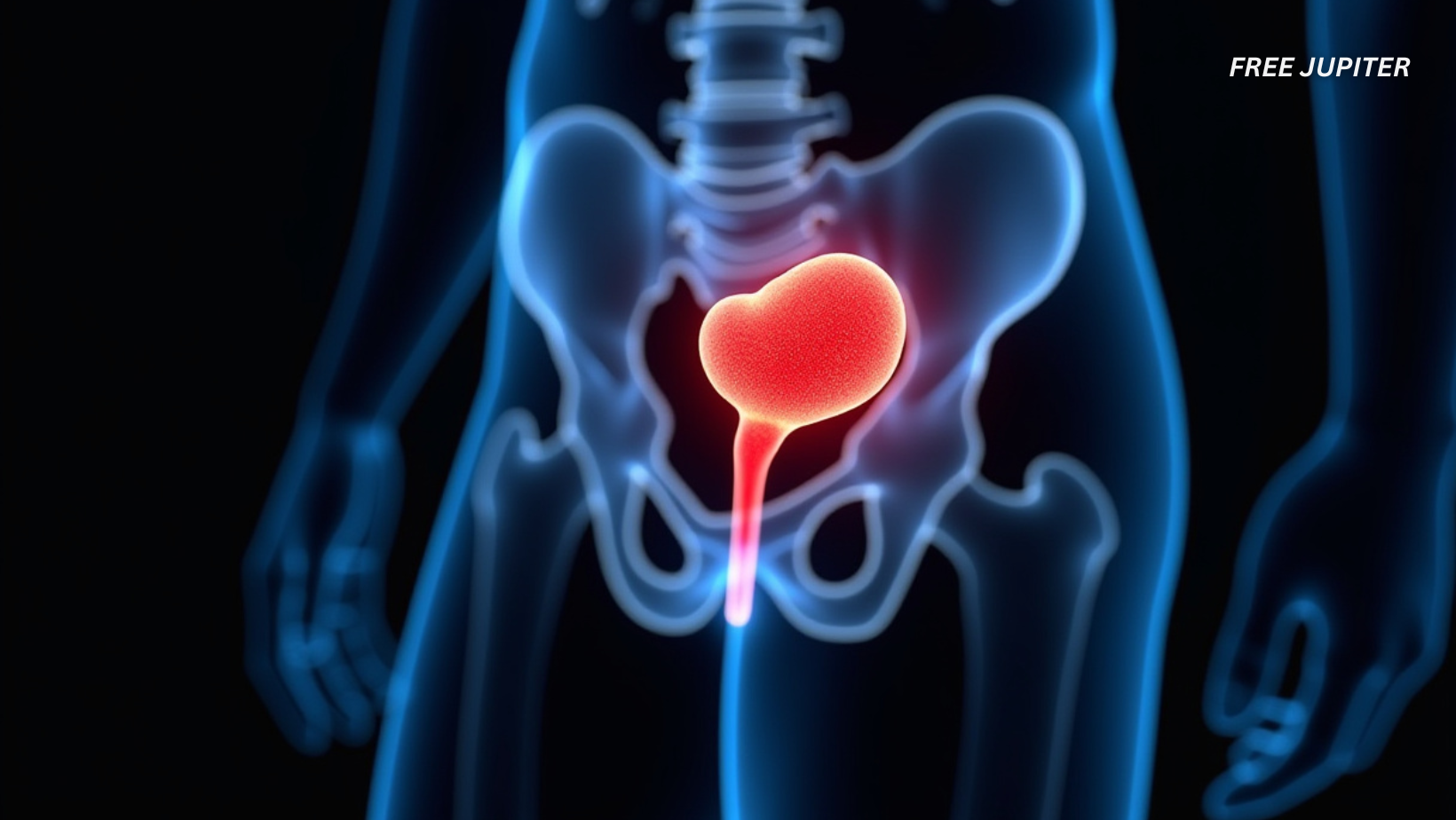
Recent studies have highlighted a startling discovery: men who neglect one crucial habit may face a significantly heightened risk of prostate cancer. This increase in danger has caught the attention of health professionals, who are eager to share insights that could potentially save lives.
The American Cancer Society notes that roughly one in eight men will confront a prostate cancer diagnosis at some point. It currently stands as the second leading cause of cancer-related deaths in men, falling only behind lung cancer. Though approximately one in 44 men will ultimately lose their battle with this disease, many who receive early diagnoses survive and continue to thrive. The key difference often lies in early detection.
Health experts are sounding alarms over one practice men tend to overlook — skipping regular prostate cancer screenings. By missing these appointments, men could be raising their risk of death from prostate cancer by as much as 45 percent. This simple step, often ignored or postponed, might be the difference between life and death.
Nationally implemented screening protocols, particularly those utilizing prostate-specific antigen (PSA) testing through blood analysis, could offer a critical advantage. Detecting the cancer at its earliest stages opens the door to timely treatment, drastically improving outcomes. The research supporting this claim is both vast and compelling.
Data collected over the last 20 years by the European Randomized Study of Screening for Prostate Cancer (ERSPC) paints a clear picture. This extensive study, drawing information from seven European countries and involving tens of thousands of men, consistently points to the lifesaving potential of PSA screenings. According to the ERSPC, regular screenings can slash the risk of dying from prostate cancer by around 20 percent.
Despite the wealth of evidence, a worrying trend has emerged. Fewer men are attending these crucial consultations. This drop in attendance has been linked to a corresponding rise in the likelihood of death from prostate cancer. The contrast between those who attend and those who do not is both stark and alarming.
The research, spearheaded by scientists from the Erasmus MC Cancer Institute at the University Medical Centre in the Netherlands, involved a sample group of 72,460 men. The findings were clear. Approximately one in six men were categorized as non-attenders, having missed every scheduled appointment. These individuals faced a 45 percent higher risk of death from prostate cancer when compared to their counterparts who attended screenings.
Read more: Cancer Rates Are 82% Higher In Young Women Than In Men: ‘Something Broader Is Going On’
Men who did participate in screenings saw tangible benefits. Their risk of dying from prostate cancer dropped by 23 percent. On the flip side, those who skipped appointments faced a 39 percent higher likelihood of death. This pattern of avoidance, experts believe, could be rooted in a broader tendency to shy away from healthcare and preventive measures.
Dr. Renée Leenen, the study’s lead author and a respected expert from the Erasmus MC Cancer Institute, offered her thoughts on these findings. She suggested that those who miss screenings may be ‘care avoiders’ — individuals who generally neglect preventive health care and other beneficial practices. In contrast, men who prioritize screenings often lead healthier lifestyles and remain vigilant about their well-being.
According to Dr. Leenen, understanding these behaviors is crucial. Healthcare professionals need to delve deeper into why certain men opt out of screenings. Gaining this understanding could pave the way for more effective population-based prostate cancer screening programs, designed to encourage participation across all demographics. Increasing attendance, she believes, could play a pivotal role in the success of national screening initiatives.
The data and conclusions from this research are set to be shared at the upcoming European Association of Urology (EAU) Congress in Madrid, Spain. The presentation aims to shed light on these pressing issues and inspire actionable change across Europe and beyond.
For men, the message is simple but vital. Regular screening can save lives. Prostate cancer, when caught early, is far more manageable. The consequences of avoidance can be tragic.
Interestingly, the correlation between healthcare habits and cancer mortality rates goes beyond mere attendance. Men who are proactive in other aspects of their health — such as maintaining a balanced diet, exercising regularly, and managing stress — are more likely to attend screenings. This cumulative effect reinforces the idea that good health practices often go hand-in-hand.
A reluctance to visit the doctor may be attributed to fear, denial, or simply a busy lifestyle. Unfortunately, these reasons can lead to dire outcomes. Healthcare providers are urged to not only offer accessible screening programs but also to focus on education. Raising awareness about the importance of early detection could encourage more men to make their health a priority.
Read more: Specific Protein Found To Keep Cancer Cells Dormant: Study
Programs tailored to address these barriers could revolutionize prostate cancer outcomes on a national scale. Flexibility in scheduling, outreach in communities where healthcare avoidance is common, and targeted messaging can all make a difference.
Moreover, PSA screening itself has evolved. Previously, some skepticism existed regarding overdiagnosis and unnecessary treatments. However, recent advancements in screening methods and follow-up care have mitigated many of these concerns. Today’s protocols are more refined, aiming to balance the benefits of early detection with the risks of overtreatment.
Doctors now have more tools at their disposal to differentiate between slow-growing cancers that may never cause harm and aggressive forms that require immediate attention. These improvements make PSA screenings even more valuable.
In addition to PSA tests, other diagnostic tools and techniques have been developed. MRI scans and biopsies, for instance, offer additional layers of accuracy in diagnosis. Combined, these approaches enhance the chances of identifying cancers that genuinely need intervention.
The psychological aspect of screening cannot be overlooked. Men who participate in these health checks not only gain peace of mind but also strengthen their relationship with healthcare providers. This rapport can foster an environment where questions are welcomed, and concerns are addressed early.
For those hesitant to undergo PSA testing, healthcare professionals recommend starting with open conversations. Discussing family history, lifestyle factors, and individual risk can help men make informed decisions about their health.
Prostate cancer, while serious, is not always an immediate death sentence. Many cases progress slowly, and when caught early, patients have a range of treatment options. Surgery, radiation, hormone therapy, and active surveillance are among the common approaches. Each case is unique, and medical teams work closely with patients to choose the best course of action.
The financial burden of late-stage cancer treatments can be enormous. By contrast, early detection and intervention often result in simpler, less invasive treatments and better quality of life. On a broader scale, national screening programs could save healthcare systems billions of dollars while saving countless lives.
Read more: Vitamin K Precursor Found To Destroy Cancer Cells In New Scientific Breakthrough
Family members also play a crucial role. Loved ones can encourage men to prioritize their health and attend regular screenings. Support systems make a tangible difference in health outcomes.
Communities, too, can foster a culture of health awareness. Local initiatives, informational seminars, and public health campaigns all contribute to higher attendance rates at screening appointments.
In conclusion, the message from experts is clear and urgent. Regular prostate cancer screenings are not just a recommendation — they are a lifeline. The risk of ignoring these appointments is simply too great. Men are encouraged to take charge of their health, make time for screenings, and remain vigilant.
Healthcare systems are urged to make screenings more accessible and to understand the barriers that prevent men from attending. Education, outreach, and compassion can turn the tide, saving lives in the process.
As the findings of this comprehensive study prepare to be unveiled to the world, one hope remains constant: that more men will hear the call and act on it. Prostate cancer can be fought — but only if men take that crucial first step toward early detection.